Types of Telemedicine: Benefits, Types, and Examples
Quick Summary: There are various types of types of telemedicine. Store-and-forward allows data sharing for later analysis. Real-time interaction enables instant communication. Remote patient monitoring tracks health conditions remotely. Examples of real time telemedicine include virtual consultations, remote monitoring devices, and specialist collaboration, enhancing healthcare accessibility and efficiency.
Introduction
The way you deliver services is very crucial in the healthcare sector. It explains value, efficiency, and the treatment you offer your patients. Now, healthcare software provides three main types of telemedicine services.
Each of these has its advantages when you correctly use them. It could benefit both providers and receiving parties. Hence it could enhance patient engagement, better access to medical history, and medical access to people that do not hold insurance.
After the covid 19 hit the world, many healthcare organizations and medical professionals have turned to telehealth technologies more. It was a great tool to bridge the physical gaps. But the question is, what will virtual care look like after a pandemic? Telemedicine makes care more accessible to people who might have access issues and makes it more convenient for staff and patients.
Therefore this article will explain the main types of telemedicine. It will also provide examples of telemedicine solutions for both delivering and receiving parties. Let’s get started!
Define Telemedicine services
Telemedicine provides virtual services using technological devices such as mobiles and computers. Most of the time, telemedicine tends to use live video conferencing. But on the other hand, many prefer phone consultations or email messaging.
Also, people contact their family doctors virtually to avoid physical location contact. While some specialists have full-fledged telemedicine apps. Here are some reasons why both doctors and patients can use different types of telemedicine apps:
- To check whether the patient needs in-person treatment
- Facilitate particular types of medical care like mental health treatment or assessing minor infections
- Prescribe some new medicines or renew it
- Provide therapies like physical therapy
Telemedicine is an excellent tool for medical and other health care professionals to maintain physical distance during treatment. Healthcare organizations can easily use telemedicine to access a patient’s medical history and deal with chronic diseases.
What are the main types of telemedicine?
Real-time interactive telemedicine
Real-time interactive services are provided to the users through video chat, messaging apps, or other communication modes. And through two-way communication, a provider may assist a person in getting medical care, even over a phone call. The only difference is that the traditional in-person visits with real-time telemedicine.
It is a telemedicine type used mainly by physicians and psychiatric evaluations. Hence it can help you seek care at the right time, like in an emergency when high blood pressure or blood sugar rises. It is also an excellent technology for follow-ups and medication oversight.
To best use the telehealth industry, the healthcare industry must ensure that all medical communications are done through HIPAA-compliant telemedicine platforms. Therefore it is illegal to use all messaging platforms for private practice.
Benefits of Real-time interactive telemedicine
One of the many benefits of real-time interactive services is live consultations. Patients can seek quality services online just as they get them in person.
Patients do not have to wait longer and stay in waiting rooms. With the help of telehealth technology, physicians can provide a faster diagnosis by connecting with patients at the mentioned time.
With telehealth technology, there is no need to visit healthcare facilities. Patients that reside in rural areas or those that face disabilities can find this technology to be a good choice.
If you are a specialist, you can easily book appointments with people across the licensed region. Hence you will not have to serve only your locality. Many platforms have booking pages where practitioners can manage their schedules.
As live consultations include talking with patients and physicians, they can establish an emotional connection. Hence this can boost the loyalty of patients.
Store-and-forward telemedicine (asynchronous video)
Store and forward is one among the types of telemedicine that is also known as asynchronous telemedicine. It is a type of telemedicine that depends on transferring health data among patients and doctors. This data can include laboratory reports, images, sounds, and much more. Also, to ensure that private data is safe, it should be transferred securely.
Store and forward telemedicine focuses on storing telemedicine data securely and forwarding them to make a treatment plan. It is an approach that enhances efficiency. Hence when patients from different regions come together with their opinions, it could lead to better treatment. All the principles are followed while organizations implement internal electronic health records systems.
The benefits of store-and-forward telemedicine
Employing store-and-forward telemedicine substantially enhances the caliber of healthcare services and elevates patient encounters. This streamlined process also fosters expedited patient outcomes, leading to swifter and improved patient results.
Patients are no longer required to arrange appointments and endure waiting times for an extra specialist consultation to access their examination outcomes. Instead, they can conveniently receive their test results electronically, directly from their computer, utilizing a swift, uncomplicated, and user-friendly procedure.
During the collaborative process of diagnosing a patient, specialists can share information at their convenience. It eliminates the necessity for simultaneous meetings among general practitioners, specialists, lab reports and patients. Once the medical records have been distributed to the primary physician and all relevant parties, each individual can review and analyze the patient and medical records themselves at their convenient moment.
Medicaid and Medicare offer extensive coverage across numerous regions, and many states provide healthcare insurance to their residents. For certain marginalized groups, government funding represents the sole avenue to access medical services.
By employing store-and-forward telemedicine, healthcare professionals can gather patient information, analyze data, and arrive at well-informed diagnoses. This technology simplifies storing and retrieving a patient’s health records, making them readily available whenever needed.
Remote patient monitoring (telemonitoring)
Remote patient monitoring software involves patients utilizing wearable devices such as heart monitors, skin patches, smart shoes, or smartwatches to gather essential health data. This information is transmitted to device applications, which relay it to a cloud-based telemedicine server.
Healthcare providers and remote nursing services supervise patient records and analyze this data. Occasionally, patients might manually measure their vital signs instead of relying on automated trackers. For example, patients could use a specialized test kit to monitor their glucose levels.
Typically, remote monitoring is employed for patients managing chronic conditions like diabetes, asthma, or cardiovascular disease. It’s also a prevalent method for remotely monitoring individuals or patients recently discharged. It further promotes greater access to medical history and information sharing at distant sites.
Benefits of remote patient monitoring
Remote patient monitoring relies on collecting original medical data through wearable devices, empowering healthcare practitioners to make well-informed, data-driven decisions. The accuracy of vital records also contributes to an enhanced recovery rate.
Physicians gain the advantage of receiving health data without needing an in-person visit, enabling them to review and process it at their convenience. This flexibility empowers physicians to structure their workdays efficiently according to their pace.
While a significant portion of medical data is now collected autonomously, specific essential metrics require patient self-monitoring. When physicians equip patients with the necessary tools, they can actively participate in their healthcare journey, improving their healthcare experience.
Telemedicine, as opposed to conventional stationary treatment, allows individuals to remain in their homes while being remotely supervised by healthcare providers, thereby potentially reducing costs associated with in-person care.
Read more: Patient Journey Management Software: Why Hospitals Need It
What are the Benefits of Telemedicine?
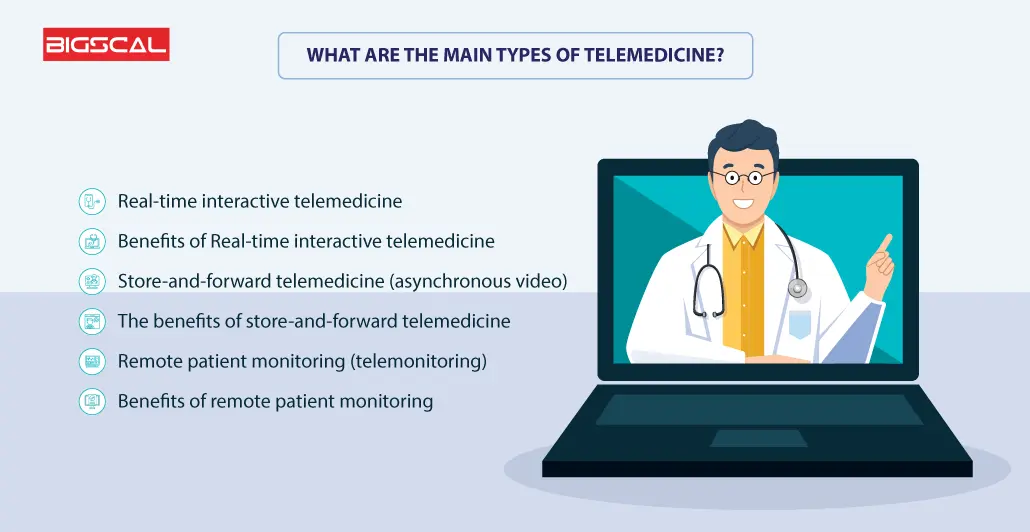
Benefits for patients
Lower costs:
Many pieces of research suggest that people who employ telemedicine tend to spend less time in the hospital. Hence it further helps them in cost reduction and saves them from spending unnecessary time.
Enhanced healthcare accessibility:
Telemedicine enhances healthcare accessibility for individuals with disabilities and other groups, such as older adults, those facing geographical isolation, and individuals in correctional facilities.
Promotion of preventive care:
Telemedicine facilitates more accessible access to preventive care, improving long-term health. This benefit is particularly significant for individuals facing financial or geographical challenges in obtaining quality healthcare.
For example, a 2021 study revealed the effectiveness of preventive telehealth services for elderly individuals in high-income countries, highlighting the need for advancements in low and low-middle-income countries.
Convenience:
Telemedicine offers the convenience of seeking medical care from the comfort and privacy of one’s home. It eliminates the need for taking time off work or making childcare arrangements.
Reducing infection transmission:
Traditional visits by patients to a doctor’s office involve close contact with potentially ill individuals, posing a heightened risk, especially for patients with underlying health conditions or weakened immune systems. Telemedicine reduces the risk of patients acquiring infections within a healthcare facility setting.
Benefits for healthcare providers
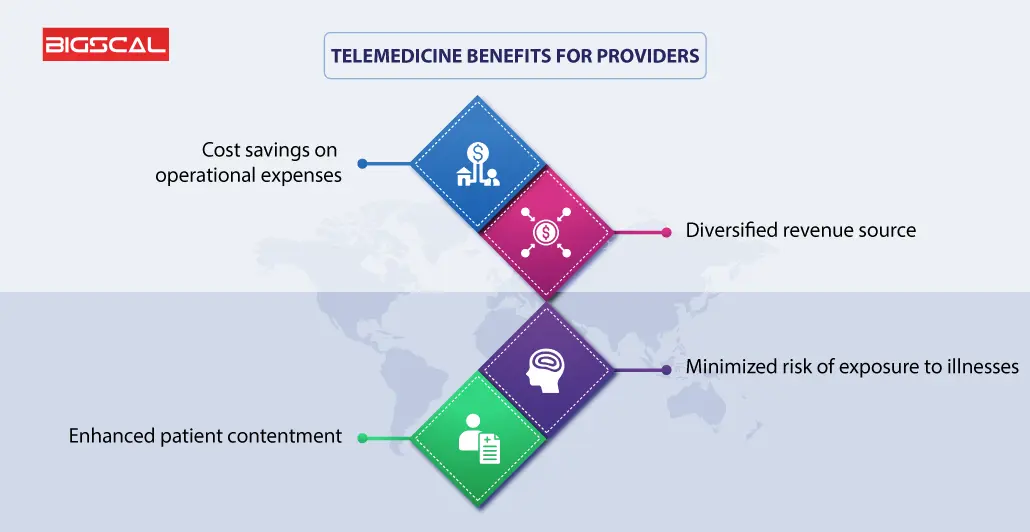
Cost savings on operational expenses:
Healthcare providers adopting telemedicine services can experience reduced overhead expenditures. It could involve decreased spending on front desk support or the opportunity to optimize office space with fewer examination rooms.
Diversified revenue source:
Medical professionals might discover that telemedicine is an additional revenue stream, enabling them to extend their care to a more extensive patient base.
Minimized risk of exposure to illnesses:
By remotely attending to patients, healthcare practitioners can avoid potential exposure to pathogens and chronic diseases that patients might carry.
Enhanced patient contentment:
Eliminating the need for patients to commute to the office or endure extended waiting times can lead to heightened satisfaction with their healthcare provider, ultimately enhancing the overall patient experience.
Read more: When Was Telemedicine Invented? History Of Telemedicine
What are the Examples of Telemedicine?

Welcoming patients to a care facility through digital front doors
It is an era where people can easily book a flight or hotel from their phones. Hence how can health systems remain behind? It could be a tiring activity to pick up the phone and set up an appointment. Healthcare facilities are continuously trying to catch up. Hence, you now have online tools to schedule meetings in your free time. Along with this, they can optimize staff and experts available at consultations.
After scheduling appointments with medical professionals, digital patient engagement can help them through the journey. It can also minimize the chances of the patient not attending a meeting.
The no-show cases of patients in radiology are about 7%. Hence this could lead to delays in diagnosis and treatments. It could also lead to financial loss of $1 million. During the pandemic, healthcare organizations have used text messages as patient reminders. Also, many have set up a virtual check-in process with text messages. Staff could receive a text message via EHR to ensure patient safety. Hence virtual waiting rooms are evolving to become the new normal.
Screening and engaging patients remotely before they enter a care facility
There are many examples of telehealth services whose usage increased after the pandemic, but the most prominent one is patient screening and engagement even before the patient avails it.
After Covid-19 hit, hospitals and organizations have tried asking questions online to assess and monitor Corona patients online. Healthcare workers contacted high-risk patients remotely to seek their medical history and data before referring them to any doctor. Hence this helped them to prevent health systems from unnecessary risks while using basic patient information, and minimum resources.
No matter whether the safety risks will lessen in health services after the pandemic, there are several other reasons why screening and medical imaging should be done online. Convenience, better patient engagement, and fewer hospital stays are some of those many benefits.
Remote patient monitoring is an added advantage after hospital discharge. Patients may be able to return home earlier to recover in the comfort of their homes.
Supporting the acquisition of medical images remotely
In addition to patient-provider telehealth tools, there has been a significant rise in provider-to-provider telehealth over the past year. This trend enables healthcare professionals to collaborate effectively even when physically separated. One notable example is the Radiology Operations Command Center, which empowers experienced imaging technologists to guide and support colleagues in remote locations during patient scans. This real-time collaboration ensures consistent image quality, minimizing the need for unnecessary repeat scans.
Furthermore, this virtual hub-and-spoke model improves access to advanced medical imaging and technologies such as MR and CT at more convenient locations and times. As a result, patients have a greater chance of receiving prompt diagnosis and treatment, regardless of where they are located.
Keeping a caring eye on patients with wearable biosensors
What lies ahead for remote patient monitoring? Look to wearable biosensors to play a significant role. These discreet chest-worn sensors can capture and transmit vital signs, including respiratory data, heart rate, posture, and activity levels.
Post the initial COVID-19 outbreak and its associated PPE shortages, hospitals have found wearable biosensors highly valuable for monitoring patients in dedicated COVID-19 units, minimizing staff exposure. However, their potential goes further, from low-acuity hospital environments to people’s homes.
For instance, a new wearable sensor in the Netherlands has been introduced to help physicians closely monitor patients transitioning from hospital to home. This sensor relays relevant health data every 5 minutes over 14 days.
In the long run, wearable biosensors could support the remote monitoring of chronic conditions such as COPD as healthcare shifts towards home-based care. The advantages are evident: improved patient comfort, reduced care costs, and the opportunity to identify patient deterioration earlier, potentially avoiding unnecessary hospital readmissions.
How does Bigscal help in telemedicine app development?
Bigscal Plays is a provider of custom telemedicine software solutions. With our expertise, we ensure seamless integration of essential features like real-time video consultations, secure patient data storage, and user-friendly interfaces.
Our proficiency in developing robust backend systems guarantees smooth communication between healthcare professionals and patients. Bigscal’s solutions encompass HIPAA-compliant security measures, safeguarding sensitive medical information.
Telemedicine apps can offer remote diagnosis, treatment, and monitoring through our technology while maintaining a high standard of user experience and data protection. In essence, Bigscal empowers the creation of efficient, secure, and user-centric telemedicine applications.
Conclusion
In conclusion, the diverse landscape of telemedicine brings forth many benefits, various types, and compelling examples that highlight its transformative potential in modern healthcare. There are different types of telemedicine solutions, each with its uses.
By breaking down geographical barriers, enhancing accessibility, and enabling remote consultations, telemedicine stands as a powerful tool in providing quality medical care. Its spectrum of types, including real-time interactions, asynchronous communication, remote monitoring, and mobile health applications, cater to various healthcare needs.
With successful instances like virtual visits, remote patient monitoring, and online consultations, the evolution of types of telemedicine exemplifies its capacity to revolutionize healthcare delivery, offering a glimpse into a more connected and patient-centered future.
FAQ
Are there different types of telemedicine?
Telemedicine can be categorized into various types based on the services provided, such as synchronous (real-time) and asynchronous (store-and-forward) telemedicine, remote monitoring, and mobile health applications.
What are the five methods of telemedicine?
The five telemedicine methods include:
- Real-time audio and video consultations.
- Store-and-forward communication (asynchronous).
- Remote patient monitoring.
- Mobile health apps.
- Online patient portals.
What are the different types of telemedicine, and how are these used?
Telemedicine comes in different forms: real-time video consultations connect patients and doctors instantly; storing and forwarding involves sharing of medical records and data at an additional time; remote monitoring tracks a patient’s health condition and health data from a distance; mobile health apps provide health information through smartphones, and online portals facilitate communication and appointment scheduling between health professionals.
What are the three components of telemedicine?
The three key components of telemedicine are the patient (or user), the healthcare provider, and the communication technology that enables remote interaction and information exchange.
What is a specific type of telehealth?
One specific type of telehealth is “remote patient monitoring,” where patients’ vital signs and health data are collected from a distance using various devices and then transmitted to healthcare providers for assessment and intervention.